What is prostatitis? In the article of a doctor with 28 years of experience, urologist, we will analyze the causes of the occurrence, diagnosis and treatment methods.
Definition of the disease. Causes of the disease
ProstatitisIs an inflammatory process of prostate tissue, accompanied by pain in the lower back, perineum or pelvic region, as well as dysfunction of the lower urinary tract.
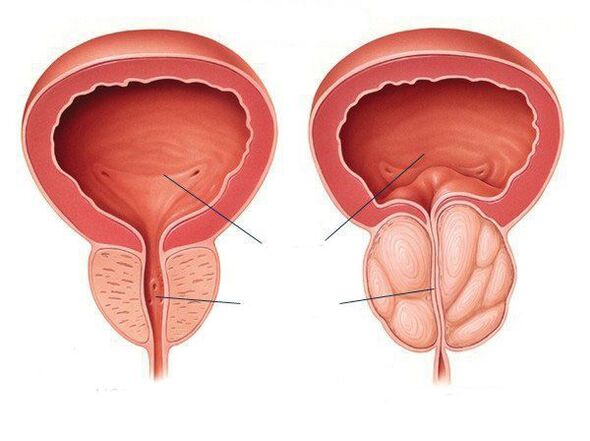
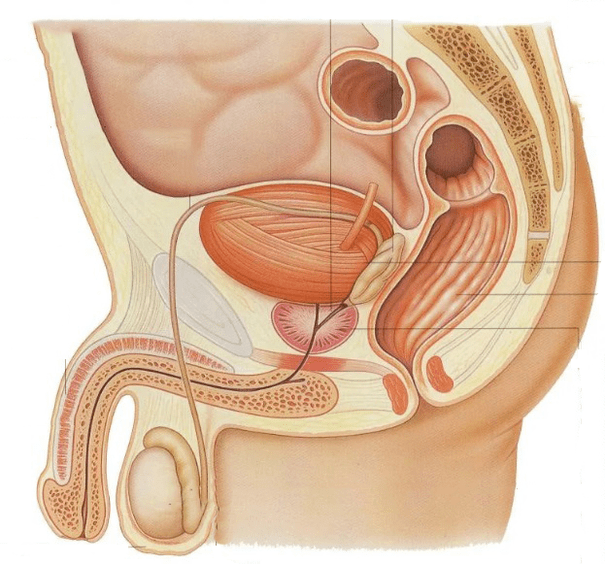
The prostate gland (prostate) refers to the male reproductive system. It sits in front of the rectum, below the bladder and is surrounded by the urethra (urethra). This is why when the prostate gland becomes inflamed, it compresses the urethra, which in turn causes various problems related to urination. The main function of the prostate is to produce a secretion (fluid) that is part of the sperm and becomes liquid to ensure the normal movement of sperm.
Abnormal conditions of the prostate gland, such as cancer or benign hyperplasia, are more common in elderly patients. Prostatitis differs in that it affects men of all age groups, but is most commonly found in men of reproductive age (8 to 35% of cases).
Prostatitis most often occurs in the practice of a urologist. It can occur suddenly (acute) or gradually and its manifestations are permanent and long-term (chronic). The chronic form is much more common than the acute. Chronic prostatitis ranks fifth among the twenty most important urological diagnoses.
Prostatitis can be an independent disease or combined with benign prostatic hyperplasia and prostate cancer. Recent years have seen a decrease in the incidence of prostatitis in the male population: if in 2012 the population was 275 out of 100 thousand, then in 2017 the primary incidence was 203 per 100 thousand population.
Causes of prostatitisAre bacterial (infectious) and non-bacterial (non-infectious).Infectious prostatitisMost often in men under 35 years of age. Most often this form of the disease is caused by gram-negative microorganisms, especially enterobacteriaceae, E. coli, sera, Pseudomonas and Proteus, as well as sexually transmitted infections such as gonococcus, chlamydia, etc. Sh. Very rarely, prostatitis can occur before Mycobacterium tuberculosis. In chronic bacterial prostatitis, the range of pathogens is wider and may include atypical pathogens. We must remember that chronic bacterial prostatitis is a polyetiological disease, ie it can have several causes.
Factors contributing to the development of inflammationIn the prostate gland:
- Sexually transmitted infections;
- Immunodeficiency conditions;
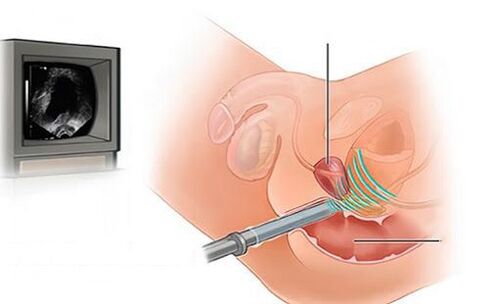
- Prostate biopsy;
- Invasive manipulations and operations;
- lifestyle;
- Diarrhea, constipation;
- Homosexual contacts;
- Frequent change of sexual partners;
- Sedentary lifestyle and a. Sh.
Chronic nonbacterial prostatitisIt is diagnosed in patients who complain of chronic pain around the prostate and the infectious (bacterial) cause of the disease is not found in them. Despite many studies, the cause of this type of chronic prostatitis is still unclear, although there are several factors that may lead to its development:
- Increased prostate pressure;
- Muscle pain in the pelvic region;
- Emotional disorders;
- Autoimmune disorders (antibodies that are supposed to fight infection, sometimes for some reason attacking prostate gland cells);
- Physical activity;
- Irregular sex life;
- Weight lifting and a. Sh.
In some cases, prostatitis may occur after transurethral procedures such as urethral catheterization or cystoscopy, as well as after transrectal biopsy of the prostate.
Although the true cases of different types of prostatitis have not been definitively established, the following data are given:
- Acute bacterial prostatitis accounts for about 5-10% of all cases of prostatitis;
- Chronic bacterial prostatitis - 6-10%;
- Chronic non-bacterial prostatitis - 80-90%;
- Prostatitis, including prostatodynia (neurovegetative disorders of the prostate gland) - 20-30%.
If you notice similar symptoms, consult your doctor. Do not be self-employed - it is dangerous for your health!
Symptoms of prostatitis
All forms of inflammationThe prostate gland, in addition to being asymptomatic, is associated with the following symptoms:
- Pain in the lumbar region;
- Feelings of discomfort with intestinal peristalsis;
- Pain in the perineum or pelvic region;
- Disorders of the lower urinary tract.
The main symptoms of lower urinary tract in the presence of prostatitis:
- Frequent urination;
- Difficulty urinating, i. e. weak flow and need for "tension";
- Burning pain or its intensification during urination.
In diagnosed menAcute bacterial prostatitisPelvic pain and urinary tract symptoms such as increased urination and urinary retention are found. This can lead to the development of systemic manifestations such as fever, chills, nausea, vomiting and weakness. Acute bacterial prostatitis is characterized by an acute onset of the disease having a clear clinical picture. This is a serious disease.
Diagnosed menChronic bacterial prostatitisNote the symptoms of a periodic nature that increase and decrease. Exacerbation is marked by pain and discomfort. The pain sensations are localized mainly at the base of the penis, around the anus or above. Also, pain can occur above the pubic bone or in the lower part of the spine, spreading to the penis and testicles. Defecation also becomes painful. Sometimes signs of infection of the lower urinary tract develop: burning pain and frequent urination, frequent urination. These symptoms can be confused with the manifestations of acute bacterial prostatitis, but it usually has a sudden onset, chills, fever, weakness, pain throughout the body, lower back, as well as in the genitals, frequent and painful urination, pain with ejaculation. If you find such symptoms, you need to see a doctor immediately.
If a standard modern examination has not established that chronic pain is caused by a pathological process in the prostate gland, then we are dealing with chronic non-bacterial prostatitis, also called.Chronic pelvic pain syndrome(The term has been used since 2003). In the presence of chronic pelvic pain syndrome, the quality of life of men is significantly reduced, as sometimes this syndrome leads to various psychological and sexual disorders:
- Increased fatigue;
- To be unable to be;
- Erectile dysfunction;
- Painful ejaculation;
- Pain after sexual intercourse and a. Sh.
Chronic non-bacterial prostatitis / chronic pelvic pain syndrome causes persistent discomfort or pain in the lumbar region, more often at the base of the penis and around the anus, for at least 3 months. Painful sensations are localized in one "target organ" or in several pelvic organs. Most often, in this form of prostatitis, the pain is localized in the prostate gland (46%).
Sexual disorders in chronic prostatitis have a number of peculiarities. First, all components of male copulation (sexual) function are violated to varying degrees: libido, erection, ejaculation. Second, sexual dysfunction is mainly found in individuals with a long (more than 5 years) history of the disease. Third, sexual dysfunction is often the main reason for finding medical help.
Erectile dysfunction is noted in 30% of patients with chronic prostatitis, which is mainly due to a psychogenic factor - a catastrophic perception of the disease.
Symptoms of prostatitis occur at least once in a lifetime in 50% of men.
Pathogenesis of prostatitis
The mechanism of development of prostatitis is multifaceted and very complex. Many factors are involved in its development. Most cases of acute bacterial prostatitis are caused by a cascade of processes caused by ascending urethral infection or intraprostatic reflux (urinary retrograde).
Microorganisms can enter the prostate gland by ascending (via the urethra) or transrectally lymphatically. Diarrhea and constipation associated with impaired rectal barrier function are considered to be a provocative factor in chronic prostatitis. However, the mechanism of penetration of microorganisms into the prostate has not yet been established.
Urinary disorders with prostatitis can lead to:
- Increase the smooth muscle tone of the prostate urethra by increasing the activity of adrenoceptors;
- Enlargement of the prostate or narrowing of the urethra, resulting in turbulent movement of the urine, obstruction of the bladder outlet, and intraprostatic reflux.
In the future there will be disruption of the drainage system of the prostate ducts, stagnation of prostate secretion, edema, activation of the arachidonic acid cascade, inflammation and ischemia. A vicious circle of pathological changes is formed.
Classification and developmental stages of prostatitis
There are 4 main categories (types) of prostatitis.
- Acute bacterial prostatitis(I category).
- Chronic bacterial prostatitis(Category II).
- Chronic nonbacterial prostatitis / syndromeChronic pelvic pain (III category). It can be inflammatory (III category A) or non-inflammatory (III category B).
- Asymptomatic inflammatory prostatitis.Histological prostatitis detected by prostate biopsy (category IV).
Chronic bacterial prostatitisUnlikeSpicy,Manifests as recurrent episodes of exacerbation, including the presence or absence of complete remissions. The symptoms are usually less severe than in acute prostatitis.
American National Institutes of Health Classification. . .
- Type I(Acute Bacterial Prostatitis) - Acute Prostate Infection: Symptoms of the disease appear suddenly. Chills, fever, pain throughout the body, weakness, pain in the lumbar and genital area, frequent, painful urination, pain during ejaculation. Potential symptoms of acute bacterial prostatitis include blood in the urine and / or semen. It is rare. It is effectively treated with antibiotics.
- Type II(Chronic bacterial prostatitis) - Chronic or recurrent infection of the prostate gland: The symptoms are the same as in acute prostatitis, but appear gradually and are less pronounced. Several courses of antibiotic therapy may be required.
- Type III(Chronic nonbacterial prostatitis and chronic pelvic pain syndrome): No confirmation of infection.
- Type IIIPresence of leukocytes in ejaculate / prostate secretion / after third prostate massage.
- III B typeAbsence of leukocytes in ejaculate / prostate secretion / third part of urine after prostate massage. Pain in the lower back and around the genitals, frequent urge to urinate, difficulty urinating (often at night), burning or painful urination, and ejaculation. Represents about 90% of all cases of prostatitis. There are no known causes or clinically approved treatments.
- Type IV(Asymptomatic Inflammatory Prostatitis): Occasionally an increase in white blood cells. No treatment is required. Revealed on prostate biopsy.
The boundaries between different forms of prostatitis are blurred.
Complications of prostatitis
With inflammatory lesions of the prostate gland, nearby organs are involved in the pathological process: testicular tuberculosis, Cooper glands, testicular vesicles, and posterior urethra. The infection can simultaneously penetrate the prostate gland and surrounding organs.
Vesiculitis- Inflammation of the seminal vesicles. The pain is localized in the groin area and deep in the pelvis, radiating to the groin. The pain is usually unilateral as both testicles are affected to varying degrees. Vesiculitis may be asymptomatic. The only complaint of patients may be the presence of blood in the semen. Periodic pyuria (pus in the urine) and pyospermia (pus in the ejaculate) are also noted.
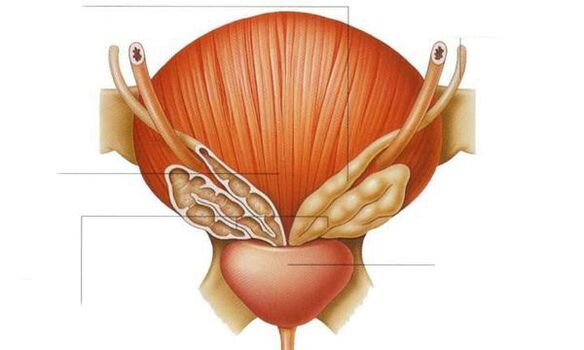
Posterior urethritis, coliculitis (inflammation of the testicles). . . Infection with prostatitis reaches the testicles, this is due to the proximity to the ducts of the prostate gland.
Prostate abscess.Pathogens that cause prostatitis can also provoke prostate abscess. It is an acute septic (bacterial) disease accompanied by weakness, fever, chills with sweating. In some cases, dementia and delirium are noted. The patient needs to be hospitalized.
Prostate sclerosis (fibrosis).It is a late complication of prostatitis based on the replacement of prostate tissue scars (connective tissue degeneration, or sclerosis), leading to the fact that the gland shrinks, shrinks in size, and completely loses its function. Typically, sclerotic symptoms develop long after the onset of the inflammatory process in the prostate gland.
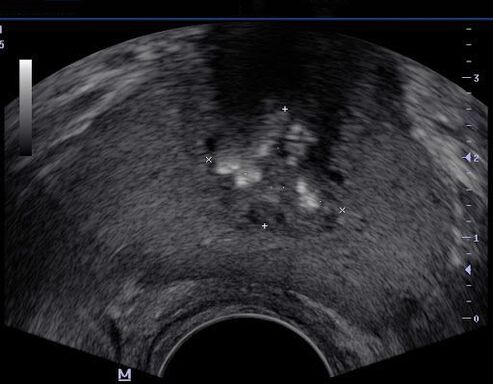
Prostate cysts.These growths can promote the formation of stones in the prostate gland. The presence of an infection in the cyst can lead to a prostate abscess. Using ultrasonography it is not difficult to diagnose prostate cyst. They can also be detected by digital examination of the rectum.
Prostate stones.They are quite common. The causes of the disease are completely unclear, but most experts agree that they arise as a result of a prolonged inflammatory process in the prostate gland. The stones are single and multiple with a diameter of 1 to 4 mm. Large stones are rare. The stones suffocate the gland, causing the secretion to stay in it, the gland stretches and separate cysts form in which the infection enters. Patients with stones in the prostate gland have to deal with constant dull pain in the perineum. Painful sensations spread to the area of the penis and cause a frequent urge to urinate, which becomes difficult and painful.
Infertility.Chronic long-term prostatitis primarily reduces the motor function of the sperm, making them completely immobile. One of the consequences is a disruption of their production, the production of immature sperm, which have a pathologically altered form (and they have a smaller number than before).
Ejaculation disorders.All forms of prostatitis cause sexual dysfunction. Initially, patients experience premature ejaculation, have a normal erection, which then weakens and the degree of orgasm decreases. Prolonged existence of chronic prostatitis helps to reduce the production of male sex hormones and weaken libido.
Erectile dysfunction.The relationship between chronic prostatitis / chronic pelvic pain syndrome and erectile dysfunction has been described. This disorder is especially painful for men.
Diagnosis of prostatitis
The appearance of the first signs of inflammation of the prostate gland requires immediate medical attention. The urologist excludes many diseases that have similar manifestations and determines which category (type) the disease belongs to. Before choosing a treatment, the specialist will conduct the necessary examinations and offer to undergo an evaluation test.
What questions can the doctor ask
At the appointment, the doctor must specify: the duration of clinical manifestations of the disease, the location and nature of the pain, for example, in the perineum, scrotum, penis and inner thigh; Changes in the nature of sperm (presence of pus and blood).
On admission the urologist will offer you to fill out special questionnaires, including the Chronic Prostatitis Symptoms Index.
The patient should ask the doctor questionsAbout what tests and studies are needed, how to prepare for them, what treatment plans to schedule and where I can get more information about the disease.
Chronic bacterial prostatitis is diagnosed when symptoms persist for at least three months.
The study includes:
- Digital examination of the rectum to determine the extent of prostate enlargement and its consistency.
- Prostate, urine and / or ejaculate secretion tests.
- Identification of urogenital infection.
- Ultrasound examination of the urinary system (kidneys, prostate, bladder to determine residual urine).
- Urine dynamics.
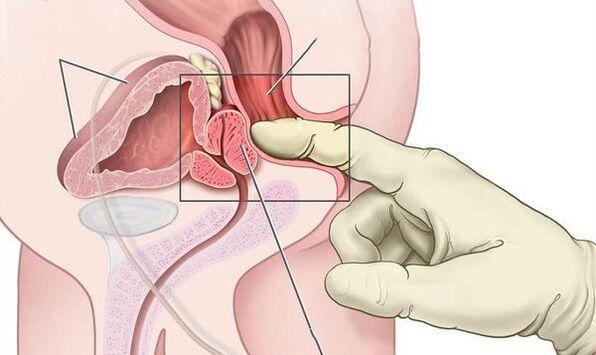
In the case of acute bacterial prostatitis, the swollen and painful prostate gland can be seen by digital examination of the rectum. Prostate massage is contraindicated as it can cause bacteremia and sepsis.
The most important study in the examination of patients with acute bacterial prostatitis is the culture of prostate secretion. To categorize chronic prostatitis, quantitative culture and microscopy of urine samples taken after prostate massage and prostate secretion are still important methods.
Androflora - A comprehensive study of microbiocenosis of the genitourinary system in men by PCR. Allows you to determine the qualitative and quantitative composition of the microflora. It is used to diagnose and treat inflammatory infectious diseases of the genitourinary system.
After determining the cause of the disease, your doctor will recommend a course of treatment. It should be remembered that standard methods can only detect infection in 5-10% of cases, which eventually leads to prostatitis.
What is the link between prostatitis, prostate specific antigen (PSA) and prostate cancer
Measurement of total PSA and free PSA levels during prostatitis does not provide additional diagnostic information. It is known that in 60 and 20% of patients with acute and chronic bacterial prostatitis, the level of prostate specific antigen (PSA) increases, respectively. After completion of treatment, PSA levels decrease in 40% of patients. PSA is not considered a specific sign of prostate cancer because PSA levels may be elevated in benign prostatic hyperplasia and prostatitis.
Treatment of prostatitis
A leading role in the treatment of pathology is assigned to drug therapy.
Treatment with alpha 1-blockers
Alpha1-blockers are prescribed for patients who complain of difficulty urinating. These medications help ease urination and relax the muscles of the prostate gland and bladder. Some patients are prescribed medications to reduce hormone levels, which can help shrink the gland and reduce discomfort. Muscle relaxants can help relieve prostate swelling, which puts pressure on the muscles. Nonsteroidal anti-inflammatory drugs (NSAIDs) can help with pain.
Standard antibiotic therapy in most cases does not reduce the number of relapses of the disease and therefore an integrated approach is often used and also prescribedAids: Biostimulants, extracts of various plants and insects and their biological components, which may be in the form ofRectal suppositories. . . Despite the large arsenal of medicines, the effectiveness of their use remains insufficient.
Physiotherapy in the treatment of prostatitis
Physiotherapeutic methods can be used for chronic prostatitis of categories II, III A and III B:
- Massage of the prostate gland (prostate);
- Laser therapy;
- Microwave hyperthermia and thermotherapy;
- Electrical stimulation by modulated currents in skin or rectal electrodes;
- acupuncture (acupuncture).
The efficacy and safety of this treatment are still being studied. It is also used to treat prostatitisFolk methods, for exampleHirudotherapy.The effectiveness and safety of this method in the treatment of prostatitis have not been proven.
Stem cell injection
Cell therapy (stem cell injections) in the treatment of prostatitis is currently a promising technique in the early stages of development. At this time, regarding the injection of stem cells into the prostate, we can only have hypotheses about its mechanisms, as well as empirical data obtained by separate groups of researchers.
Surgical treatment of prostatitis
Surgical methods are used only to treat complications of prostatitis - abscesses and testicular blisters.
Treatment of chronic pelvic pain syndrome requires separate consideration. Asymptomatic inflammatory prostatitis (category IV) should not be treated unless the patient intends to undergo prostate surgery. In this case, the patient undergoes a prophylactic course of antibiotic therapy.
Diet and lifestyle for prostatitis
A special diet for prostatitis is not necessary, but eating lots of vegetables, lean meats and dairy products will improve bowel function. It is important to get a sufficient amount of fiber, foods rich in vitamin E (wheat germ, corn oil, etc. ), sugar should be replaced with natural honey. Proper nutrition of prostatitis can improve bowel function and reduce the likelihood of recurrence or speed recovery. It is recommended to follow a healthy lifestyle, get more fluids and limit caffeine and alcohol.
Forecast. Prevention
Acute prostatitis often occurs with chronic, even timely and adequate treatment.
Complete recovery is not always possible, however with the right consistent therapy and following your doctor’s recommendations it is possible to eliminate discomfort and pain. IndependentTreatment of prostatitis at homeCan be dangerous and cause complications.
Not all cases of prostatitis can be defined as the cause, but there are a few steps you can take to prevent prostatitis. The same steps will help you control your existing symptoms:
- Drink plenty of fluids. Intake of large amounts of fluid causes frequent urination, which helps to release infectious agents from the prostate urethra.
- Empty the bladder regularly.
- Avoid irritating the urethra. Limit caffeine, spicy foods and alcohol.
- Reduce prostate pressure. Men who frequently ride bicycles need to use a split seat to relieve pressure on the prostate area.
- Be sexually active.




























