Prostatitis is an inflammatory process associated with inflammation of the prostate gland (prostate) in men. This disease is most common in men over the age of 30 years. This disease causes pain in the lumbar, perineum or pelvis, is accompanied by disruption of the normal process of urination and in severe forms causes erectile dysfunction and serious problems in the relationship with a partner.
About a quarter of cases among infertile couples are due to a male factor that affects the inability to conceive. Male infertility is a violation of the quality of sperm and their quantitative content in the ejaculate.
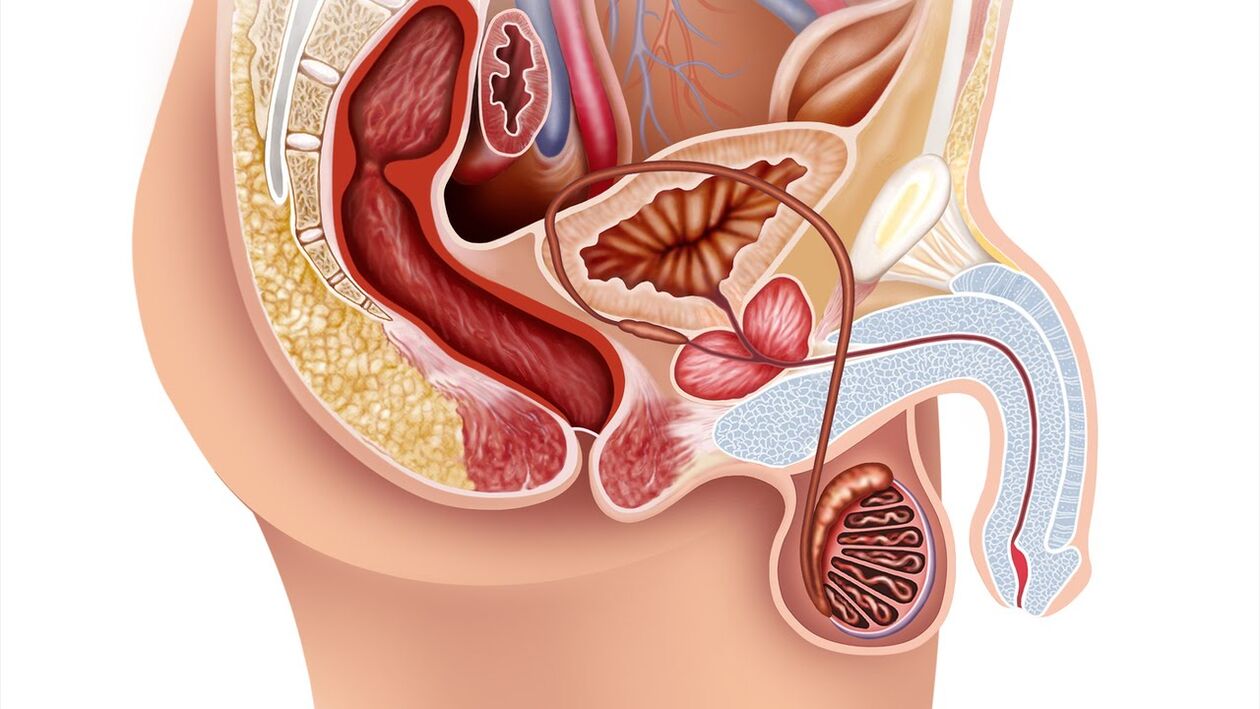
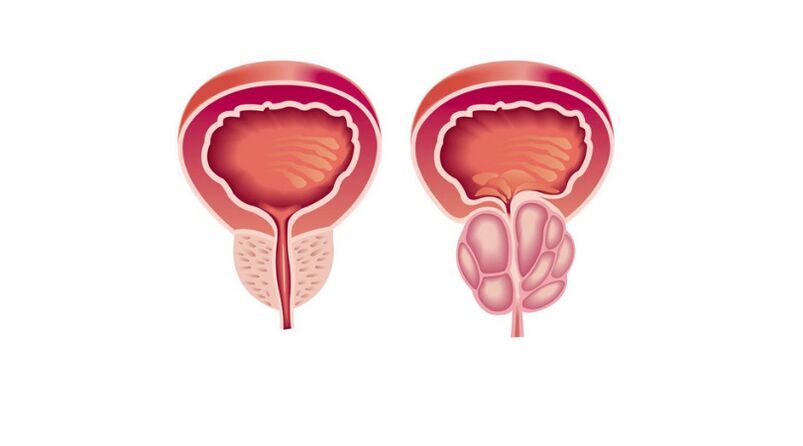
The prostate gland (prostate) refers to the male reproductive system. It has the shape of a chestnut, is located in front of the rectum, under the bladder and surrounds the urethra (urethra). When the prostate gland is inflamed, it contracts to the urethra, which in turn causes urinary problems. The main function of the prostate is to produce a secretion (fluid) that is part of the sperm and mixes it, which ensures the normal movement of sperm.
Prostatitis is very common in urologist practice. It can occur suddenly or gradually, appearing constantly and for a long time (chronic prostatitis). The chronic form of this disease is more common than the acute one. Chronic prostatitis ranks fifth among the twenty major urological diagnoses.
Since prostatitis is an active focus of infection in the body, it requires mandatory treatment, even if its symptoms do not bother you.
Causes of prostatitis
The list of reasons for provoking inflammation of the prostate gland is very diverse:
- Diseases of the genitourinary system (cystitis, urethritis, pyelonephritis);
- Sexually transmitted infections (trichomoniasis, gonorrhea);
- Infections associated with pneumonia, influenza, tonsillitis, furunculosis;
- Chronic constipation that forces a man to strain regularly;
- Sedentary lifestyle and irregular sex life leading to secret stagnation;
- Urinary retention - a swollen bladder increases pressure on the prostate;
- Frequent hypothermia (or overheating);
- Injuries to the pelvis;
- Hormonal disorders that weaken the immune system.
Very often prostatitis is caused by pyogenic microbes: E. coli, streptococci and staphylococci, mycoplasmas, Candida fungi, Trichomonas, tuberculosis bacilli. They multiply very quickly and destroy the prostate tissue, which manifests itself in inflammation.
In most cases, the onset of prostatitis provokes an infection that reaches the prostate gland through the urethra. It happens that it enters the body through the blood or lymph, passes through the bladder or rectum.
ᲛImportant! Decreased immunity is very dangerous for a patient with chronic prostatitis, since the prostate gland quickly becomes inflamed with fatigue, stress, insomnia, malnutrition and other harmful factors.
With a sedentary lifestyle and lack of constant sex life, the blood supply to the pelvic organs deteriorates, leading to oxygen starvation and swelling of the prostate tissues. The stagnant secretion is an ideal environment for the growth of pathogenic microorganisms that cause inflammation.
Types and forms of prostatitis
Prostatitis, depending on the cause of the disease, is divided into types and forms:
By type, they are distinguished:
Bacterial prostatitis- Inflammation caused by infection. Bacterial prostatitis is found in both young and older men.
Congestive prostatitis- Inflammation caused by stagnation of secretion. It develops in men with sedentary lifestyles who do not have a regular sex life. This form can quickly add to the infection, and then the stagnation process is complicated by the bacterial form.
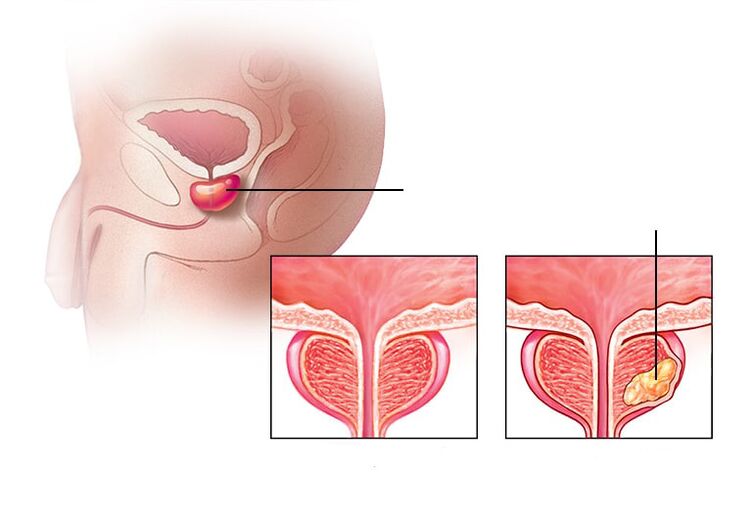
Calculus prostatitis- Stones form in the prostate gland. Untreated chronic prostatitis can lead to this complication. This disease affects older men who do not follow the advice of a urologist.
Depending on the shape of the stream:
Acute form of prostatitis- It is an inflammation of the prostate gland caused by an infectious agent, characterized by the appearance of swelling and purulent foci in the tissues. 30-58% of men of reproductive age (30-50 years) face such a diagnosis.
Chronic form of prostatitisCharacterized by persistent or recurrent urogenital symptoms caused by a bacterial infection in the prostate gland. The chronic form accounts for 10% of all cases of prostatitis.
Symptoms of prostatitis
GeneralSymptoms of prostate inflammationthey are:
- Pain in the lumbar region;
- Sensations of discomfort during bowel movements;
- Pain in the perineum or pelvis;
- Disorders of the lower urinary tract.
Acute stage of prostatitis is accompanied by general intoxication syndrome. This disease is characterized by a sharp manifestation of symptoms with a clear clinical picture:
- A sharp rise in body temperature, chills, nausea, vomiting and weakness;
- Pain syndrome and chills in the joints and muscles;
- Increase in the size of the prostate and the appearance of discomfort in the perineal area;
- Frequent urination and urinary retention.
In the background of individual inflammatory processes may develop purulent-septic disease, which affects the blood. In such a situation the patient should be hospitalized immediately: treatment of prostatitis with sepsis should be carried out exclusively in the clinic.
AtChronic prostatitis of bacterial natureSymptoms are usually absent, so treatment is started only when an infection in the genitourinary system is detected, which is manifested against the background of complication of the disease. In this case, you can observe:
- Pain during ejaculation;
- The appearance of blood in the ejaculate;
- The presence of discharge from the urethra;
- Erectile dysfunction may develop.
If the examination did not show that chronic pain is caused by prostate gland pathologies, then we are dealing with this case.Chronic nonbacterial prostatitisOr e. წChronic pelvic pain syndrome. With this disease, the quality of life of men is significantly reduced, as it leads to various disorders of psychological and sexual nature:
- Increased fatigue;
- Feeling of helplessness;
- Erectile dysfunction;
- Painful ejaculation;
- Pain after sexual intercourse and a. Sh.
Similar symptoms may be related to other urological diseases, so it is impossible to diagnose prostatitis with symptoms alone. For example, urinary incontinence and pain are found in prostate adenoma, cystitis, various oncological tumors of the urogenital organs, etc. Sh.
Diagnosis of prostate inflammation
After the first signs of inflammation of the prostate gland, the patient should immediately consult a doctor - urologist. The doctor should rule out many diseases that have similar manifestations and determine which disease they belong to.
To confirm that the patient has no other diseases (eg, appendicitis, oncology, inflammatory processes of the bladder and kidneys, prostate adenoma), the doctor should conduct the necessary examinations:
- Collecting anamnesis (questioning the patient);
- General inspection;
- Rectal examination;
- To study the secrets of the prostate gland;
- Analysis of sexually transmitted infections;
- Ultrasound examination of the prostate, scrotum and pelvic organs.
At the appointment, the urologist should explain to the patient the duration of clinical manifestations of the disease, the localization and nature of pain (for example, in the perineum, scrotum, penis and inside the thigh), the characteristic changes in sperm (presence of pus and blood).
Your doctor will diagnose chronic bacterial prostatitis with symptoms lasting at least three months.
The survey includes:
- Digital rectal examination of the gland to determine the degree and consistency of prostate enlargement.
- Prostate secretion, urine and / or ejaculation tests.
- Identify urogenital infection.
- Urodynamic research.
- Ultrasound examination of the genitourinary system (kidneys, prostate, bladder) to determine residual urine.
- Cultural study of prostate secretion and microscopy of different parts of urine and prostate secretion.
- Androflora is a comprehensive study of microbiocenosis of the urogenital tract in men by PCR, which determines the qualitative and quantitative composition of the microflora.
Once the cause of the disease is determined, the doctor will prescribe a course of treatment. It should be remembered that standard methods can detect infection only in 5-10% of cases, which eventually leads to prostatitis.
The patient must undergo a thorough diagnosis as the success of the treatment will depend on the accuracy of the results.
Treatment of prostatitis
When a urologist has diagnosed, determined the cause and form of prostatitis, he or she should prescribe treatment.
Drug therapy plays a leading role in the treatment of this disease:
Antibacterial therapy
In the first stage of therapeutic therapy it is necessary to eliminate the inflammation. Antibiotics are the mainstay of treatment for acute bacterial prostatitis and are recommended for chronic bacterial prostatitis. The doctor chooses the antibacterial drug depending on which bacteria caused the disease. The patient will have to take a course of oral antibiotics for 4-6 weeks. Eliminating chronic or recurrent prostatitis takes more time. Hospitalization may be required for very severe manifestations where an intravenous course of antibiotics is administered. Usually, this occurs during acute bacterial prostatitis.
Treatment with alpha1-blockers
When you have difficulty urinating, your doctor will prescribe alpha1-blockers to help you urinate and relax your prostate and bladder muscles. Muscle relaxants will relieve the pain caused by the swelling of the prostate gland, which puts pressure on the neighboring muscles. Nonsteroidal anti-inflammatory drugs will help relieve the painful syndrome.
Also, your doctor may prescribe auxiliary drugs: biostimulants, extracts of various plants and insects in the form of rectal suppositories. Unfortunately, the use of drugs alone in the treatment of prostatitis remains insufficient.
The principles of sequence of actions must be observed in the treatment of this disease. Treatment of prostatitis is always complex.
Physiotherapy for the treatment of prostatitis
In the categories of chronic prostatitis you can additionally use physiotherapy methods:
- Prostate gland massage (prostate);
- Laser therapy;
- Microwave hyperthermia and thermotherapy;
- Electrical stimulation by modulated currents with skin or rectal electrodes;
- acupuncture (acupuncture).
Alternative methods such as hirudotherapy (treatment of medical puppies) are sometimes used to treat prostatitis, but the effectiveness and safety of this method have not been proven.
Stem cell introduction
Cell therapy (stem cell injections) is a promising method of treating prostatitis today, it is in the early stages of development. As for the insertion of stem cells into the prostate, there can only be hypotheses about its mechanisms and empirical data obtained by separate groups of researchers.
Surgical treatment of prostatitis
Surgical methods are used to treat complications of prostatitis (abscess and abscess of the testicles).
Treatment of chronic pelvic pain syndrome requires separate consideration. Asymptomatic inflammatory prostatitis does not require treatment.
Diet and lifestyle during prostatitis
Prostatitis does not require a special diet, but eating large amounts of vegetables, lean meats and dairy products will help improve bowel function. It is necessary to enrich the body with a sufficient amount of fiber, foods rich in vitamin E (wheat germ, corn oil, etc. ), replace sugar with natural honey. Proper nutrition with inflammation of the prostate gland will help improve bowel function and reduce the likelihood of recurrence or accelerate recovery. The patient should limit coffee intake, exclude alcohol, drink plenty of fluids and follow a healthy lifestyle.
Preventive measures to prevent prostatitis
When a man leads the right way of life: keeps proper nutrition, walks in sports, then the chances of developing his chronic prostatitis are very small. Abandoning bad habits and casual sex is the prevention of this disease.
ᲛImportant! There is primary and secondary prevention to prevent the development of prostatitis in men.
Primary- Aims to prevent the emergence of disease. It is about a balanced diet, physical activity regime, timely treatment of any infectious disease of the body and regular sexual intercourse, etc. Sh.
secondary- Aims to prevent recurrence of existing chronic prostatitis and provides regular examination and prophylactic treatment by a urologist with multivitamins, remedies and sports.




























